Regulation of Alzheimer's disease amyloid-beta formation
Regulation of Alzheimer's disease amyloid-beta formationAlzheimer's Donation
Donate Online Now
.

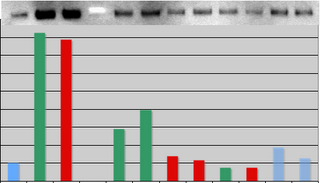
lzheimer's disease (AD) is associated with accumulation of the neurotoxic peptide amyloid-beta (A), which is produced by sequential cleavage of amyloid precursor protein (APP) by the aspartyl protease beta-secretase and the presenilin-dependent protease gamma-secretase. An increase of casein kinase 1 (CK1) expression has been described in the human AD brain. We show, by using in silico analysis, that APP, beta-secretase, and gamma-secretase subunits contain, in their intracellular regions, multiple CK1 consensus phosphorylation sites, many of which are conserved among human, rat, and mouse species. Overexpression of constitutively active CK1, one of the CK1 isoforms expressed in brain, leads to an increase in A peptide production. Conversely, three structurally dissimilar CK1-specific inhibitors significantly reduced endogenous A peptide production. By using mammalian cells expressing the C-terminal fragment of APP, it was possible to demonstrate that CK1 inhibitors act at the level of gamma-secretase cleavage. Importantly, Notch cleavage was not affected. Our results indicate that CK1 represents a therapeutic target for prevention of A formation in AD.
The studies lead author Marc Flajolet and from the Nobel Prize winning laboratory of Paul Greengard, director of the Fisher Center for Alzheimer's Disease Research at Rockefeller. "Studies of brain tissue from Alzheimer's patients have shown an increase in casein kinase 1 expression," says Greengard, Vincent Astor Professor and head of the Laboratory of Molecular and Cellular Neuroscience. "We found that the key enzymes involved in beta-amyloid production - called BACE and gamma-secretase - were targets of casein kinase 1, so we investigated what role it might be playing." The scientists modified mouse cells to generate a form of casein kinase 1 that was always active, and found that these cells produced more beta-amyloid protein than normal. Then, using three different types of chemicals, they blocked the protein from functioning. When they did this, they were able to reverse the production of beta-amyloid protein, without affecting the signaling of Notch proteins. The studies suggest that an Alzheimer's therapy based on these chemicals could reduce or halt beta-amyloid build-up without causing side effects. "Numerous efforts have been directed at the development of drugs that inhibit gamma-secretase," says Greengard, "but there have been significant side effects in animal studies. Our hope is that this research might lead to drugs that don't have those problems."